Hospitals eTool
Clinical Services » Radiology
The Radiology department performs and interprets diagnostic and interventional procedures. It provides a wide range of medical imaging procedures in general radiography and subspecialty areas. [See OSHA’s statement regarding its choice of focus points for this hospital area]
Select a common safety and health topic or hazard from the list below to view information related to the topic/hazard.
Hazards
Staff are exposed to ionizing radiation from radiation-generating devices used in diagnostic and therapeutic procedures. Examples of devices include portable and fixed X-ray machines, fluoroscopy units, and linear accelerators. Staff may also be exposed to radioactive materials, such as radionuclides used in nuclear medicine, which are regulated by the U.S. Nuclear Regulatory Commission (NRC) or an NRC Agreement State.
Exposure
Radiation dose is received when workers are near an operating radiation-generating device or a radioactive source. The dose received depends on the type of radiation, the amount of radiation generated, the duration of exposure, the distance from the source of radiation, and the amount and type of shielding in place.
Health Effects
Radiology department staff members may be repeatedly exposed to low levels of ionizing radiation over the course of their careers. Adverse health effects, such as cancer, may occur years following such exposure. The probability of an adverse health effect occurring is proportional to the radiation dose received (World Health Organization 2016).
Studies of atomic bomb survivors have shown significant associations between cancer and radiation dose levels of about 10 rems (0.1 Sv) or greater, with the cancer risk increasing as the radiation dose increases. For low-level radiation exposure (i.e., whole body doses less than about 10 rems (0.1 Sv)), statistical limitations in studies have made cancer risk assessment more difficult (National Research Council et al. 2006).
In 2006, the National Research Council's Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation reviewed the available data and concluded that the cancer risk would continue linearly at low doses. This finding means that there is likely no safe exposure level (i.e., threshold) and that even low radiation doses have the potential to cause a small increase in cancer risk (National Research Council 2006).
In addition to cancer, cataracts (i.e., detectable lens opacities) are another radiation-induced health effect that could occur in radiology staff (International Commission on Radiological Protection 2011).
For more detailed information on health effects from radiation exposure, see OSHA's Ionizing Radiation Safety and Health Topics Page.
For OSHA requirements on Ionizing Radiation (e.g., exposure limits and monitoring, posting, and recordkeeping requirements), see OSHA's Ionizing Radiation Standard (29 CFR 1910.1096).
Dose Monitoring
For OSHA requirements on personnel monitoring, see OSHA's Ionizing Radiation Standard (29 CFR 1910.1096).
In certain circumstances OSHA’s standard requires employers to provide personal dosimeters for the long-term monitoring of a worker’s radiation dose. Dosimeters include thermoluminescent finger dosimeters (TLDs), optically stimulated luminescence body (OSL) dosimeters, or film badges.

These passive dosimeters for personal exposure monitoring can be worn whenever working with radiation-generating devices, radioactive materials, or radioactive patients. Depending on the work situation, wear a body dosimeter at collar level, chest level or waist level. Wear finger ring dosimeters on the hand which is closest to the radiation source.
Personnel who work in high-dose fluoroscopy settings may be asked to wear two dosimeters for additional monitoring. Oftentimes, one dosimeter is worn on the outside of the lead apron at the collar (unshielded) and one on the inside at the waist (shielded).
Other Radiation Safety Practices
Provide radiation safety training to all workers who operate or are exposed to radiation-generating equipment, radiation sources, or radioactive materials.
Keep radiation exposures As Low As Reasonably Achievable (ALARA), and certainly below regulatory limits.

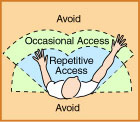
The three basic concepts of radiation protection are: (1) minimize the time of exposure, (2) maximize the distance from the source of radiation, and (3) use shielding. Applying these concepts will help to keep radiation exposures ALARA.
Some examples of radiation protective practices include:
- Using the shortest practical irradiation times.
- Equipping X-ray rooms with a barrier wall with a lead-plated window for the technician to step behind before taking an X-ray.
- Using radiation-absorbing shields such as ceiling-suspended lead shields and table-suspended drapes as barriers to protect against X-ray exposure when procedures are in close proximity to the patient.
- Providing and ensuring employees use personal protective equipment (PPE) lined with lead or lead-equivalent materials (e.g., products made from dense elements or alloys of Pb, Sb, Bi), including lead or lead-equivalent aprons, thyroid collars, leaded eyewear with protective side shields, and leaded gloves for use by workers in the X-ray field. Ensure that workers do not place their hands in the primary X-ray beam. Providing and ensuring employees use properly fitted aprons to reduce ergonomic hazards and provide optimal radiation protection (Miller et al, 2010).
- Ensuring that procedures, like those that use remote fluoroscopy, are run using controls in an adjacent room, to the extent feasible.
- Giving a specific person the responsibility for ensuring proper maintenance of portable X-ray machines. Preventive and corrective maintenance programs for X-ray machines are detailed in 21 CFR Part 1000, Radiological Health, U.S. Food and Drug Administration.
For detailed guidance on recognized practices, see:
- Federal Guidance Report No. 14. Radiation Protection Guidance for Diagnostic and Interventional X-Ray Procedures (FGR14). U.S. Environmental Protection Agency Interagency Working Group on Medical Radiation. November, 2014.
- Miller DL, et al. Occupational Radiation Protection in Interventional Radiology: A Joint Guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Cardiovasc Intervent Radiol. 2010. 33:230-239.
- National Council on Radiation Protection and Measurements (NCRP), Report No. 168, Radiation Dose Management for Fluoroscopically-Guided Interventional Medical Procedures. July 21, 2010.
- National Council on Radiation Protection and Measurements (NCRP), Report No. 105, Radiation Protection for Medical and Allied Health Personnel. September 15, 1989.
- National Council on Radiation Protection and Measurements (NCRP), Report No. 102, Medical X-ray, Electron Beam, and Gamma-ray Protection for Energies up to 50 MeV. April 4, 1989.
Note that additional controls are required for the use of radioactive materials in hospitals, as regulated by the Nuclear Regulatory Commission. See 10 CFR 20, Standards for Protection against Radiation and 10 CFR 35, Medical Use of Byproduct Material.
Additional Information
- Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII, Phase 2. National Research Council. 2006.
- Ionizing Radiation. OSHA Safety and Health Topics Page.
- Ionizing Radiation Fact Book. U.S. Environmental Protection Agency (EPA). The Offices of Air and Radiation and of Radiation and Indoor Air published this document, which includes information on the health effects of ionizing radiation.
- Ionizing radiation, health effects and protective measures. World Health Organization (WHO). April 2016.
- OSHA Technical Manual (OTM) - Hospital Investigation Health Hazards, Section VI: Chapter 1.
- Statement on Tissue Reactions. International Commission on Radiological Protection (ICRP), April 21, 2011.
- Webster, E.W. EDE for Exposure with protective aprons. Health Physics Journal 1989. 56(4):568-569.
- Memorandum of Understanding between the U.S. Nuclear Regulatory Commission and the Occupational Safety and Health Administration. OSHA, (September 6, 2013). Clarifies areas in which each Agency has jurisdiction.
Hazards
Radiology staff that frequently lift and reach for patients and equipment during X-ray procedures and/or patient transfers may experience work-related musculoskeletal disorders (MSDs) (e.g., strain and sprain injuries to back and shoulder areas). Note also that prolonged use of lead aprons can result in back and neck pain.
- Transporting Patients and Equipment
-
Some radiology tasks increase the amount of push or pull force that the radiology staff must exert when moving patients or equipment from one area to another. An increase in force exertion may increase the risk of injury to the back, legs and shoulders.
Hazards
- Exerting force in awkward postures, such as bending or reaching, due to handles or push points that are too high or too low.
- Any unexpected, abrupt stoppage or deceleration when moving equipment, resulting in the use of excessive force and awkward body postures. This can occur when (for example):
-
Wheels are the wrong size for the transitions between flooring types or rooms.

- Wheels are too small to easily pass over gaps between elevator and main floor.
- Wheels (casters) are poorly maintained or are inappropriate for the flooring surface.
- Obstructions are placed in the line of travel.
- The floor is damaged.
- Debris is left on the floor.
-
Recognized Controls and Work Practices
- Use smaller, handheld equipment to perform bedside studies, whenever it is available and appropriate.
- Use mechanical-powered assist devices whenever large or heavy patients or equipment must be moved for longer distances.
-
Ensure that equipment has the appropriate wheels (casters) to facilitate safe transport over all flooring and room conditions.

- Generally, wheels that have a larger diameter, a narrower width and are made of a harder material will traverse gaps and changes in flooring more easily, reducing the necessary push force.
- Swivel casters are recommended when maneuvering in tight locations. Note: Ensure that at least one set of casters is lockable to provide improved inline steering.
- Ensure that all equipment is maintained according to established schedules and that all employees understand the procedure for reporting damaged equipment.
- Ensure that the controls for equipment are easily accessible without bending or reaching. Applicable controls may include controls that allow selection between two-wheel, four-wheel and braked positions and controls for central locking (which provides greater stability to the equipment).
- Ensure that radiology equipment is pushed or pulled from the side where handles are placed.
- Ensure that floors are clean and free of debris that may cause the wheels to get stuck while in motion.
- Ensure that aisles are kept open and free of extraneous items such as gurneys, wheelchairs or other carts.
- Ensure that employees are aware of the procedures to report damage to flooring and walkways.
-
Train radiology staff on safe and appropriate use of equipment when moving patients, wheelchairs, beds, stretchers and other radiology equipment, including training on the following practices:

- Push instead of pull. Lean slightly into the load to let your body weight assist with force exertion.
- Push at about chest height.
- Push smoothly and slowly to start.
- Do not bend or twist while exerting force.
- Keep wrists straight.
- Keep elbows close to the body.
- Develop work schedules to minimize the time lead aprons are worn without a break.
Additional Information
- Improving Patient and Worker Safety: Opportunities for Synergy, Collaboration and Innovation. The Joint Commission.
- Guidelines for Nursing Homes: Ergonomics for the Prevention of Musculoskeletal Disorders. OSHA Publication 3182, (2003, Revised March 2009). Section III, Identifying Problems and Implementing Solutions for Resident Lifting and Repositioning, includes an assessment of resident handling tasks that can help to determine the safest methods for performing necessary tasks for individual patients without injuring workers. A list of sample equipment solutions for patient lifting and repositioning tasks is also included.
- Ergonomics Safety and Health Topic Page. OSHA.
- Inspection Guidance for Inpatient Healthcare Settings. (June 25, 2015). OSHA memorandum establishing guidance for inspections conducted in inpatient healthcare settings.
- Also see Hospital-wide Hazards - Work-related Musculoskeletal Disorders.
- Transferring Patients to and from the Imaging Table
-
Radiology staff may need considerable support and assistance to move patients onto or off of imaging tables.
Hazards
- Pushing or pulling to position beds, gurneys and wheelchairs as part of the patient transfer process can require exertion of significant force, especially when dealing with bariatric (obese) patients, carpeted floors or poorly maintained wheels and casters.
- Assuming awkward postures such as bending, twisting or reaching when moving patients from wheelchairs, beds or gurneys to the imaging table. Awkward postures, especially when combined with the exertion of force, increase the risk of injury to the back, shoulders, and lower and upper extremities.
- Using significant force when lifting bariatric patients from wheelchairs, beds or gurneys increases the risk of injury to the back and shoulders.
Recognized Controls and Work Practices
Safe Patient Handling Programs and policies that limit or prohibit manual lifting have been shown to be effective in reducing MSDs in hospital and nursing staff. Research has shown that the use of mechanical lifting equipment and a Safe Patient Handling Program can significantly reduce injuries to hospital staff.
Minimize manual lifting of patients in all cases and eliminate manual lifting when possible. Focusing solely on “proper body mechanics" during lifting is not sufficient to prevent MSDs.
- Use mechanical powered transfer devices such as lifts or hoists to move patients (especially bariatric or non-ambulatory) from wheelchairs, beds, or gurneys.
- Use an air mattress or other appropriate transfer aid for lateral patient transfers between the gurney and examination table.
- When appropriate, use multi-use devices such as chairs that can open up into beds. These allow patients to move from a sitting position to a prone position without transfer.
- Use additional employees to assist in moving and transferring equipment or patients if:
- A mechanical powered device is not available.
- Awkward postures would otherwise result.
- Push force exceeds about 50 pounds.
Additional Information
- Worker Safety in Hospitals: Caring for Our Caregivers – Safe Patient Handling OSHA.
- Safe Patient Handling. OSHA Safety and Health Topics page.
- Safe Patient Handling: Preventing Musculoskeletal Disorders in Nursing Homes. OSHA Publication 3708, (February 2014).
- Also see Hospital-wide Hazards - Work-related Musculoskeletal Disorders.

Hazard
Employees who use a computer intensively (e.g., at the remote radiology computer workstation, or for data entry) are at increased risk for developing musculoskeletal disorders (MSD) of the hand/arm, shoulder, neck, and back.
Recognized Controls and Work Practices
Look at the workstation layout and:
- Arrange materials and supplies in front of the body so that they can be easily reached with the elbows in, close to the torso.
- Provide adjustable, supportive padded chairs that support the forearms, legs, and low back. The proper height of the arm-rests allows the elbows to hang normally at the side of the body.
- Arrange monitor so that the most commonly viewed area is slightly below (about 20 degrees) horizontal eye level and can be seen without looking up, or leaning forward.
- Provide engineering controls to limit awkward positions (e.g., provide headsets for employees to use when answering phones).
- Use a keyboard that includes an adjustable mouse support that can be easily reached from a keying position. Employees need to keep wrists straight while typing and use wrist pads to rest on when not typing.
Repetitive Motions during hand-intensive tasks: Performing hand-intensive tasks (such as data entry, word processing) with a bent wrist creates considerable stress on the tendons and their sheaths as they are bent across the harder bones and ligaments that make up the outside structure of the wrist.


- As the fingers are activated, the tendon slides through the sheath and over the hard parts of the bent wrist, pinching the sheath between the tendon and these hard entities.
- Repetitive finger activations in these postures can create wear and tear on the tendon and the sheath.
- Prolonged forceful finger exertions in these postures can stretch and fray the tendon and create contact trauma to the sheath.
This wear and tear, fraying, or contact trauma can create irritation and swelling that may lead to tendonitis, tenosynovitis, and potentially carpal tunnel syndrome.
Additional Information
- For more information, see OSHA's Computer Workstations eTool which can help identify, analyze and control musculoskeletal disorders in computer workstation tasks.
Workers in hospital settings may be exposed to a variety of common and emerging infectious disease hazards, particularly if proper infection prevention and control measures are not implemented in the workplace. Examples of infectious disease hazards include seasonal and pandemic influenza; norovirus; Ebola; Middle East Respiratory Syndrome (MERS), tuberculosis, methicillin-resistant Staphylococcus aureus (MRSA), and other potentially drug-resistant organisms.
Infectious diseases are caused by agents that are transmissible through one or more different routes, including the contact, droplet, airborne, and bloodborne routes. The transmission of infectious agents through the bloodborne route—a specific subset of contact transmission—is defined in the Bloodborne Pathogens (BBP) standard, 29 CFR 1910.1030 (See the Bloodborne Pathogens section below).
An effective infection control program normally relies upon a multi-layered and overlapping strategy of engineering, administrative and work practice controls, and PPE. It is OSHA's intent in this eTool to highlight some – not all – of the controls that would be necessary to the development and implementation of an effective program. Implementing the controls highlighted here alone will not typically protect workers from infection hazards.
Follow standard and transmission-based precautions to prevent worker infections (see also the OSHA page: Worker protections against occupational exposure to infectious diseases). Early identification and isolation of sources of infectious agents (including sick patients), proper hand hygiene, worker training, effective engineering and administrative controls, safer work practices, and appropriate personal protective equipment (PPE), among other controls, help reduce the risk of transmission of infectious agents to workers.
Employers must comply with the BBP standard to the extent that there is "occupational exposure" (i.e., to the extent employers should reasonably anticipate contact with blood or other potentially infectious materials (OPIM) that may result from the performance of duties). Employers must also comply with the PPE Standard, 29 CFR 1910 Subpart I, and the OSH Act's General Duty Clause, 29 U.S.C. 654(a)(1), to protect their workers from infectious disease hazards. The General Duty Clause requires each employer to "furnish to each of his employees employment and a place of employment which are free from recognized hazards that are causing or are likely to cause death or serious physical harm to his employees."
OSHA provides agent-specific guidance for a variety of pathogens that workers in hospital settings may encounter. See OSHA's Safety and Health Topics Pages for Biological Agents and Bloodborne Pathogens and Needlestick Prevention for additional information.
In this module, OSHA provides additional guidance specifically for:
- Bloodborne Pathogens (BBP)
-
Bloodborne pathogens are pathogenic microorganisms present in human blood that can cause disease in humans. These pathogens include, but are not limited to, Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), Human Immunodeficiency Virus (HIV) and Viral Hemorrhagic Fevers (e.g. Ebola). [29 CFR 1910.1030(b)]
Hazards
Exposure of radiology staff to blood or other potentially infectious materials (OPIM) during X-ray procedures or other patient care.
Requirements under OSHA's Bloodborne Pathogens Standard, 29 CFR 1910.1030
The Bloodborne Pathogens Standard requires precautions when there is occupational exposure to blood or OPIM (as defined by the standard). Under the standard, OPIM means (1) the following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids; (2) any unfixed tissue or organ (other than intact skin) from a human (living or dead); and (3) HIV-containing cell or tissue cultures, organ cultures, and HIV- or HBV-containing culture medium or other solutions; and blood, organs, or other tissues from experimental animals infected with HIV or HBV.
OSHA requires employers to ensure that the biosafety officer or other responsible person conducts an exposure determination to determine the exposure of workers to blood or OPIM throughout the hospital setting. [29 CFR 1910.1030(c)(2)(i)].
For a complete explanation, see Hospital-wide Hazards - Bloodborne Pathogens.
- Tuberculosis
-
Hazard
Exposure of radiology staff to patients with tuberculosis during x-ray procedures. Exposure may also occur after radiology procedures are completed because treatment rooms were not properly ventilated after being occupied by a patient who has tuberculosis (TB).
TB is caused by a bacterium called Mycobacterium tuberculosis and is spread by airborne droplets generated when a person with TB disease coughs, speaks, sneezes, etc. Infection occurs when a susceptible person inhales droplet nuclei containing the bacteria, which then become established in the body.
TB transmission has been documented in healthcare settings where healthcare workers and patients come in contact with people who have TB disease (see CDC Burden of TB in the United States page). An additional hazard is present because of multidrug-resistant (MDR) TB. MDR organisms are resistant to the drugs that are normally used to treat TB, such as the antibiotics Isoniazid and Rifampin (see CDC Drug-Resistant TB page).
Requirements under OSHA's Respiratory Protection Standard, 29 CFR 1910.134
Employers must comply with applicable provisions of OSHA’s Respiratory Protection standard, 29 CFR 1910.134, for using respirators to protect against TB hazards.
Recognized Controls and Work Practices
The CDC discusses three types of controls for TB infection in healthcare settings:
- Administrative controls to minimize the number of areas where exposure to TB can occur
- Environmental controls to reduce the concentration of TB
- The use of respiratory protection in situations that pose a high risk for exposure
Recognized controls and work practices include:
- Providing an area in the radiology department that is ventilated separately for TB patients (i.e., patients with suspected or confirmed TB) in facilities in which TB patients are frequently treated. If this is not possible, ensuring that TB patients wear surgical masks, stay in the radiology suite the minimum amount of time possible, and be returned promptly to their isolation rooms.
- Healthcare facilities serving populations that have a high prevalence of TB may need to supplement the general ventilation or use additional engineering controls in general-use areas where TB patients are likely to go (e.g., waiting-room areas, emergency departments, and radiology suites). These engineering controls include:
- A single-pass, non-recirculating system that exhausts air directly to the outside.
- A recirculation system that passes air through HEPA (High Efficiency Particulate Air) filters before re-circulating it to the general ventilation system.
Additional Information
- Enforcement Procedures and Scheduling for Occupational Exposure to Tuberculosis. OSHA Directive CPL 02-02-078, (June 30, 2015). Contains information concerning OSHA’s general enforcement policy and procedures for conducting inspections and issuing citations related to occupational tuberculosis (TB) hazards.
- Inspection Guidance for Inpatient Healthcare Settings. (June 25, 2015). OSHA memorandum establishing guidance for inspections conducted in inpatient healthcare settings.
- Fit Testing Requirements for Employees Who Wear Respirators to Protect against M. Tuberculosis, SARS, Smallpox, and Monkeypox. (February 5, 2004).
- Tuberculosis. OSHA Safety and Health Topics Page.
- Tuberculosis. Centers for Disease Control and Prevention.
- Lewinsohn, D.M., et al. (2017). "Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children." Clinical Infectious Diseases 64(2): e1-e33.
- Respiratory Protection Program Training and Resources. American Association of Occupational Health Nurses (AAOHN). This online training program prepares hospital staff for respiratory protection in the workplace.
- Also see Hospital-wide Hazards – Tuberculosis.

