Tuberculosis
Control and Prevention
Effective strategies for controlling and preventing worker exposure to TB bacteria depend on the risk of exposure and the work tasks performed. Appropriate precautions are critical to protect high-risk workers exposed to TB. Solutions that may be helpful in preventing TB are early identification, isolation, and treatment of people with TB.
- General Recommendations for Employers
- General Precautions for Workers
- Additional Measures for Specific Industries
General Recommendations for Employers
Conduct a job hazard analysis to identify workers at risk of exposure to TB prior to instituting control measures. Consider work operations and tasks when performing hazard analyses. Employers should develop specific work instructions to ensure procedures are consistently followed. The most effective job hazard analysis engages workers and their representatives throughout the process of their development and implementation.
Select the appropriate controls based on the results of the hazard analysis, including engineering controls, administrative controls, safe work practices, and personal protective equipment (PPE). Some controls may be required by OSHA standards.
See NIOSH's TB Health Hazard Evaluations webpage to learn whether TB health hazards are present at the workplace and recommended ways to reduce hazards and prevent work-related illness.
Personal Protective Equipment
Provide workers with appropriate PPE based on the results of the hazard analysis. PPE may include but is not limited to:
- Disposable gloves
- Protective clothing (e.g., long-sleeved coveralls with a waterproof apron [if working with elephants, for example], patient care gown)
- Disposable shoe covers or shoe covers that can be disinfected
- Safety goggles or combination of safety glasses with face shield
- Respiratory protection
If it is determined that workers need respirators, use a NIOSH-certified air-purifying respirator with a particulate filter that is rated N95 or higher. Respirators must be used as part of a comprehensive respiratory protection program that meets the requirements of OSHA's Respiratory Protection standard (29 CFR 1910.134) and includes training, medical exams, and fit testing.
See OSHA's Personal Protective Equipment Safety and Health Topics page for additional information on PPE selection and use.
Training
Train workers who may have contact with potentially infected people, laboratory specimens, elephants, or contaminated materials to understand their risk of exposure to TB based on the jobs they perform. Make sure that workers understand the controls in place and protective measures available to prevent or reduce exposure to TB in the workplace. Training should emphasize the risks posed by undiagnosed TB disease and the measures that can be taken to reduce the risk. Training should be documented and repeated as needed.
Train workers to use PPE appropriately. OSHA requires training on how to use PPE for workers who are required to use such equipment for their jobs. This training includes when to use PPE; what PPE is necessary; how to properly put on, use and take off PPE; how to properly dispose of or disinfect, inspect for damage, and maintain PPE; and the limitations of PPE. Applicable standards in 29 CFR 1910 Subpart I include those for personal protective equipment (29 CFR 1910.132), and respiratory protection (29 CFR 1910.134). OSHA offers a variety of training videos on respiratory protection.
Prevent needlesticks from needles contaminated with TB bacteria. For ways to prevent needlesticks see 29 CFR 1910.1030, Bloodborne pathogens (BBP) standard. TB is not a bloodborne pathogen, but the BBP standard can provide guidance.
General Precautions for Workers
All workers with potential exposure to TB should take the following precautions:
-
Avoid unprotected contact with potentially infected persons or elephants. When making first contact with all individuals who may have TB, visually screen for signs and symptoms of potential TB illness.
-
Provide input to employers during the development of a hazard analysis and a TB control strategy. Implement specific work instructions and mitigation strategies developed to prevent or reduce exposure to TB in the workplace.
-
Wear respiratory protection. A NIOSH-certified N95 filtering facepiece respirator or better should be worn as part of a comprehensive respiratory protection program that includes medical exams, training, and fit testing, and that meets the requirements of OSHA's Respiratory Protection standard (29 CFR 1910.134). If unable to wear a disposable particulate respirator because of facial hair or other fit limitations, wear respirators that do not require a face seal (e.g., positive pressure respirators of the hood and helmet type, or types that can be used with a continuous-flow, supplied-air respirator).
-
Participate in training on infection control procedures. Workers should be aware of potential hazards on the job and how to prevent accidental transmission. Employers should provide training on the facility's policies and procedures regarding TB. Train workers on TB procedures, aerosol treatments, power washing, and any other practices that could increase the risk of exposure.
-
Monitor health symptoms if possible exposure to TB has occurred. Workers should monitor their health for symptoms of TB infection for 10 weeks following known exposure and call their state or local health department immediately if they develop any illness signs or symptoms. Most of the signs and symptoms of TB overlap with those of other respiratory illnesses. Contact your state or local health department if you have been potentially exposed to TB; health departments want to help, even if it turns out to not be TB. If any workers have symptoms, they should stay home and limit contact with others as much as possible until the results from a TB test are known. State and local public health departments can assist in monitoring and advising when isolation is no longer required.
Additional Measures for Specific Industries
Some workers may require additional levels of protection because of the industry they work in or the job they do. These recommendations and relevant OSHA standards also provide a framework for protecting workers where OSHA or an approved State Plan do not have authority. Please note that the following recommendations are to be used in addition to the general guidance provided elsewhere in this document.
Zoo Workers
On rare occasions, zoo workers or others who have contact with infected elephants or contaminated surfaces have been infected with TB.
- Plan for TB. Develop a robust TB response and control plan and have all employees review and familiarize themselves with the plan. At a minimum, the TB control program should include the following:
-
A ventilation assessment
-
TB surveillance program and respiratory protection program
-
Sustained use of appropriate fit-tested respiratory protection (N95 respirator or equivalent or higher-level respirator) for anyone who has contact with elephants or works in their enclosure. The zoo or elephant environment may be wet and the appropriate respirator should be selected; and
-
A comprehensive employee training program.
-
-
Implement biosecurity practices and ensure workers follow those practices to prevent the introduction of TB and other diseases into elephant herds. Restrict visitors to elephant facilities. Provide workers with clean protective clothing and equipment. Institute cleaning and disinfection practices that include equipment and vehicles entering and leaving the zoo. Implement procedures to quarantine the zoo to prevent spread of disease and monitor TB exposures.
-
Ensure adequate ventilation to bring clean outdoor air into elephant enclosures, including the replacement of contaminated air and the control of any airborne contaminants. For zoos that have heating, ventilation, and air conditioning (HVAC) systems, ensure that they are operating in accordance with the manufacturer's instructions and design specifications, and conduct all regularly scheduled inspections and maintenance procedures. More information can be found on OSHA's Ventilation Safety and Health Topics Page.
Correctional Facilities
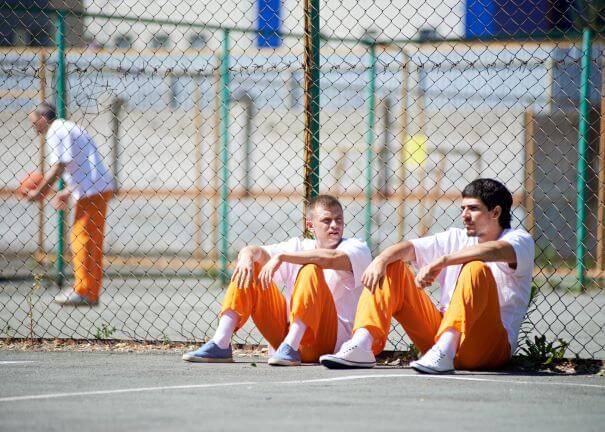
- Establish an effective TB control and prevention plan. Recommended measures in correctional facilities include:
-
Early identification of persons with active TB through entry and periodic follow-up screening
-
Successful treatment of active TB and latent TB infection
-
Appropriate use of airborne precautions (e.g., airborne infection isolation, environmental controls, and respiratory protection)
-
Comprehensive discharge planning
-
Thorough and efficient contact investigations when a TB case has been identified.
-
-
Work with state or local health departments. All TB measures in correctional facilities should be instituted in close collaboration with local or state health departments. Any TB cases should be reported to the state or local health department.
Healthcare Workers
Healthcare workers and their employers should take specific precautions to prevent the spread of TB.
-
Install and properly maintain appropriate air-handling systems in healthcare facilities. Acute care facilities should already have appropriate heating, ventilation, and air conditioning (HVAC) systems (including appropriate exhaust and filtration) to reduce the potential for exposure to airborne infectious diseases, which are appropriate for controlling TB and other respiratory diseases. See the CDC's Guidelines for Environmental Infection Control in Health-Care Facilities for detailed information on air-handling systems and other infection controls in healthcare facilities.
-
Local exhaust such as hoods, booths, or tents remove airborne contaminants at or near their source of generation. For example, booths may be required for sputum induction or other high-risk procedures that generate droplets. Booths used for source control should be instantaneously exhausted so that 100% of airborne particles are removed.
-
Place patients with suspected active TB infection in an Airborne Infection Isolation Room (AIIR). If an AIIR is not available, place a facemask on the patient (if the patient can tolerate wearing one) and isolate the patient in an examination room with the door closed. Transfer the patient as soon as possible to a facility where an AIIR is available. Negative pressure must be maintained in isolation rooms. Negative pressurization can be created in any room when exhausted air is approximately 20% greater than the rooms supplied air. Provide at least six (existing facility) or 12 (new construction/renovation) air changes per hour. The CDC's 2007 Guidelines for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings provides additional information on isolation rooms.
-
Supplemental Controls. HEPA filters may be used in general-use areas, e.g., waiting rooms and emergency rooms, when recirculating indoor air. The HEPA filter can be a portable unit or part of the centralized air-handling unit or even a whole-wall HEPA filtration unit with laminar air flow. In isolation rooms these filters can only be used as a supplemental control and are not a replacement for negative pressure ventilation.
-
UV Irradiation. These systems are optional as an additional control where exposure to TB bacilli risk is particularly high. UV radiation cannot be considered a substitute for ventilation requirements due to the low efficacy of these systems. UV may be used on recirculating air in general-use areas.
-
Implement policies and practices to minimize potential exposures. When patients with active TB are known to be admitted, airborne precautions should be implemented before arrival, upon arrival, and throughout an affected patient's presence in the healthcare setting. These patients should be placed in an isolation room with hazard signage on the door. Avoid transporting patients outside of the isolation room unless necessary, and limit the numbers of healthcare workers caring for patients and visitors allowed to see the patients. Special considerations should be employed for high-risk procedures such as cough-inducing and aerosol-generation procedures, intubation, and bronchoscopy. CDC's 2007 Guidelines for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings provides additional information.
-
Track all healthcare workers and support staff who care for or enter the rooms of confirmed or suspected active TB patients. Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations form the National Tuberculosis Controllers Association and CDC, 2019 recommends implementing a policy for healthcare workers who develop respiratory symptoms after an exposure to active TB. Workers should notify their supervisor, receive prompt medical evaluation, and comply with work exclusion (i.e., stay home) until they are no longer contagious.
For details on general enforcement policies related to occupational exposure to TB, see the OSHA Instruction: Enforcement Procedures and Scheduling for Occupational Exposure to Tuberculosis.
More information is available from the CDC's TB Infection Control in Health Care Settings and Resources for TB Programs.
More information is available from the Association for Professionals in Infection Control and Epidemiology: Tuberculosis: Considerations for an Old Threat.
Laboratory Workers
Exposure to M. tuberculosis bacteria in clinical, research, and commercial laboratory workers can occur through inhalation of aerosol droplets generated while manipulating bacterial cultures and biological specimens (blood, sputum, oral and nasal secretions, bone marrow, urine, tissues, etc.) that contain the bacteria. Aerosol-producing laboratory procedures include, but are not limited to pipetting, vortexing, centrifuging and using a syringe. Additionally, a needlestick with a contaminated needle may cause tuberculosis of the skin.
-
Refer to the U.S. Department of Health and Human Services' Biosafety in Microbiological and Biomedical Laboratories (BMBL), 6th edition for detailed guidance on biosafety controls when working with TB.
-
Use engineering controls including the use of a biosafety cabinet (BSC). Ensure that laboratory entrances and exits have self-closing doors. Conduct aerosol-generating procedures in a properly installed, maintained, and certified Class II BSC. If possible, conduct all work with infectious samples in the BSC. The OSHA Fact Sheet Laboratory Safety Biosafety Cabinets provides guidance on training and effective use of BSCs.
-
Practice Biosafety Level 2 (BLS-2) procedures for diagnostic procedures that do not produce aerosols, such as microscopic analysis of covered, stained slides. Use a Class II biosafety cabinet (BSC) for additional protection if available.
-
Use BSL-3 practices, procedures, and facilities for work involving TB bacteria, with rigorous adherence to additional respiratory protection, showering and clothing change protocols.
-
Use respiratory protection and PPE appropriate for the work tasks performed. In laboratories, the BMBL guidance can help employers select appropriate respiratory protection and PPE.
-
Perform animal work with immunocompetent rodents in an Animal BSL2 (ABSL-2) laboratory using ABSL-3 practices, while all other animal models require ABSL-3 facilities. All studies involving an airborne infection model require ABSL-3 facilities and practices.
-
Enroll laboratory workers in a medical surveillance program.
-
Minimize work tasks that contribute to the generation of bioaerosols or droplet sprays. These may include using syringes, pipetting, vortexing, centrifuging, and opening/closing sample tubes.
-
Dispose of contaminated material in appropriate biohazard containers and autoclave, incinerate, or inactivate it using an alternative method of decontamination. See the U.S. Department of Health and Human Services' Biosafety in Microbiological and Biomedical Laboratories (BMBL) for additional information on proper disinfection for TB bacteria.

