OSHA Field Safety and Health Management System (SHMS) Manual
CHAPTER 28: INFECTIOUS DISEASE AWARENESS
-
Purpose
To recognize, reduce, or prevent the spread of infectious diseases in the workplace. This chapter promotes awareness, infection control practices, and proper personal protective equipment (PPE) usage for OSHA personnel.
-
Scope
The program applies to all OSHA Personnel within a regional, area, district, or satellite OSHA office and other OSHA organizational units (i.e., Technical Center (TC) and Office of Training and Education (OTE)) covered by the OSHA SHMS Manual.
-
References
The Centers for Disease Control and Prevention (CDC) and National Institute for Occupational Safety and Health (NIOSH): Workplace Safety and Health Topics
CDC: Chain of Infection Components
CDC: Procedures for Donning and Doffing PPE
Environmental Protection Agency (EPA): Selected EPA-Registered Disinfectants
OSHA Safety and Health Topics Page: Health care: Infectious Diseases
OSHA Code of Federal Regulations: 29 CFR 1910.1030: Bloodborne Pathogens
OSHA’s Field Operations Manual (FOM) CPL 02-00-164:
Chapter 3, Section II.C, Safety and Health Issues Relating to OSHA Field PersonnelOSHA Safety and Health Management System (SHMS) Manual ADM 04-00-003, Chapters:
Chapter 2: SHMS
Chapter 7: Emergency Contingency Plan
Chapter 8: Personal Protective Equipment (PPE)
Chapter 18: Respiratory Protection
Chapter 19: Bloodborne Pathogens
Chapter 25: Medical Management
Chapter 26: Decontamination -
Definitions
Airborne Infection Isolation Room (AIIR), formerly known as a negative pressure isolation room: A single occupancy patient-care room used to isolate persons with a suspected or confirmed airborne infectious disease.
Airborne Transmission: Spreading germs through infectious droplet nuclei or particles containing infectious agents that remain suspended in air, are inhaled, enter the respiratory tract, and cause infection. See Appendix A: Guidance for Improving Air Quality in OSHA Workplaces for general information on reducing the potential for airborne transmission.
Biological Safety Cabinet Laboratory, also called a microbiological safety cabinet: An enclosed, ventilated laboratory workspace for working safely with biohazardous materials requiring a defined biosafety level.
Communicable Diseases: illnesses that spread from person to person, from animal to person, or from a surface to food. For more information on communicable diseases, see Appendix B: Spread of Communicable and Infectious Diseases.
Contact Transmission: Spreading germs by touch from direct person-to-person skin contact, animal-to-person, vector (insects to person), or transferring germs by touching contaminated surfaces. For information on how infectious diseases are spread, see Appendix B: Spread of Communicable and Infectious Diseases.
Contagious: When a disease can be spread through direct or indirect contact from one person or organism to another.
Cleaning: Use soap, water, and other cleaning agents to decrease the number of germs (i.e., viruses, bacteria, parasites, or fungi) on surfaces and reduce infection risk. Cleaning is not the same as disinfecting, see the definition of disinfecting below.
Direct Contact: A form of contact transmission through which germs are transmitted from the blood and bodily fluids of an ill (infected) person to a healthy one. Examples of direct contact include skin-to-skin touching and exposure to mucous membranes, lesions, sores, or oral secretions.
Disinfecting: Using chemicals to kill harmful germs, such as bacteria and viruses, that remain on surfaces after cleaning. Disinfecting surfaces can further lower the risk of spreading disease. Refer to EPA’s list of Selected EPA Registered Disinfectants.
Droplets: Liquid particles generated when an infected person coughs, sneezes, or talks, or during certain medical procedures, such as suctioning or endotracheal intubation. Droplets can stay in the air for prolonged periods of time and be carried on normal air currents to different spaces and areas, which can result in airborne transmission and surface contamination.
Fecal-Oral Route: Transmission of an infectious disease when food and/or water contaminated with infectious fecal material is ingested. This is a form of indirect contact. People can transmit germs to others through the fecal-oral route due to poor personal hygiene and sanitation. Transmission can also occur through direct contact with feces-contaminated body parts or airborne transmission such as a toilet plume.
Germs: See Infectious Agents definition.
Indirect Contact: A form of contact transmission through which germs are transmitted to a healthy person who touches contaminated objects such as clothing, bedding, and furniture used by an infected and contagious person.
Infectious Agents: Viruses, bacteria, fungi, protozoa, and helminths are microorganisms. Those microorganisms are the five categories of agents that cause infectious disease.
Infectious Disease: Illnesses caused by germs (see infectious agents) that enter the body, multiply, and can cause an infection and illness. For a list of infectious diseases, see Appendix C: List of Infectious Diseases and General Resources.
Infectious Disease Emergency: Circumstances that are caused by biological agents with the potential of significant illness and/or death in a population. Examples may include naturally occurring outbreaks (mumps, measles, meningococcal disease), emerging infectious diseases (SARS, pandemic influenza), and bioterrorism.
Novel Case: A case that the OSHA did not recognize or has not reasonably anticipated.
Outbreak: When three or more novel cases occur in a workplace within the time period that is consistent with the infectious disease.
Parenteral route: A type of contact transmission where germs are introduced to the body other than orally. This includes through the mucous membrane and skin punctures, piercings, bites, or cuts. For more information on sharps injuries, see 29 CFR 1910.1030: Bloodborne Pathogens.
Sanitizing: Reduces the remaining germs on surfaces after cleaning. Sanitizing is not intended to kill viruses, but disinfecting does.
Sterilizing: Gets rid of all germs (bacteria, viruses, and microorganisms) from a surface.
Vaccine: A preparation that is used to stimulate the body’s immune response against diseases and can be administered through needle injections, by mouth, or sprayed into the nose. For more information on vaccines, see Appendix D: Vaccines and Immunizations.
-
Roles and Responsibilities
- Management
- National Office
The Directorate of Technical Support and Emergency Management (DTSEM) is responsible for providing consistent guidance related to infectious disease prevention and control with consideration of the goals and mission of OSHA. DTSEM will:
- Provide technical support to the OSHA regions related to infectious diseases.
- Assist the regions in coordinating with local, state, and federal agencies to provide technical assistance and guidance related to infectious diseases.
The duties of specific offices of DTSEM to support infectious disease-related notifications/requests are as follows:
-
Office of Occupational Medicine and Nursing (OOMN) will:
- Provide support if there is a concern about an infectious disease outbreak in an area/regional office (e.g., Legionella, Norovirus, Coronavirus disease, and Hepatitis).
- Provide consultation support to the area/regional office on infectious disease precautions so that OSHA personnel can safely perform their work (selecting adequate PPE, performing contact tracing, conducting prophylaxis, etc.)
- Assist with determination of work-relatedness in the context of a case of an infectious disease in the workplace.
Note: Work-related illnesses associated with infectious diseases are reported in the OSHA Forms for Recording Work Related Injuries and Illnesses.
-
Office of Science and Technology Assessment (OSTA) will:
- Notify the DTSEM Director of any reports of work-related infectious disease cases that come from the Field offices.
Note: The Safety and Occupational Health Manager (SOHM) will provide the OSTA Director with any such reports of infectious disease cases that come from the Field offices.
- Collaborate with OOMN, Office of Emergency Management and Preparedness (OEMP), and/or Salt Lake Technical Center – Health Response Team (SLTC-HRT) and other OSHA Directorates to create and provide information that will inform OSHA Field Personnel about how to minimize their exposure to infectious diseases to reduce the likelihood of transmission.
- Collaborate with OEMP on interagency committees and workgroups related to infectious diseases.
- Collaborate with OEMP to monitor potential infectious disease outbreaks that affect the community.
- Notify the DTSEM Director of any reports of work-related infectious disease cases that come from the Field offices.
-
OSHA Technical Center – Health Response Team (HRT):
- Assist in identifying potential infectious disease hazards, routes of exposure, and controls for specific worksites and situations.
- Upon request, the HRT will analyze the existing ventilation system at worksites to determine the effectiveness of the system to perform adequately for its intended purposes.
- Provide control recommendations for Job Hazard Analysis (JHA) in novel or unusual situations.
- Support onsite inspections as needed if higher level PPE is required (Level A/B). See SHMS Chapter 8: PPE, for more information.
- Assist in identifying potential infectious disease hazards, routes of exposure, and controls for specific worksites and situations.
-
Regional Offices and Directorates:
- The Regional Administrator and Directorate Directors (as appropriate) must:
- Ensure the overall administration of the Infectious Disease Awareness program at regional and local office levels.
- Contact the SOHM when a novel case of an infectious disease outbreak is identified.
Note: The Regional Safety and Occupational Health Manager (RSHM) shall provide the Regional Administrator/Office Director with reports of reportable infectious disease exposures and incidents that come from the field offices of their jurisdiction.
- The Regional Administrator and Directorate Directors (as appropriate) must:
-
Area Offices and Technical Centers
- An OSHA Manager will notify the RSHM if a significant infectious disease hazard has been identified.
Note: OSHA Field Personnel should report any notice from local health departments regarding contact tracing or office response to a potentially infectious employee (e.g., an employee with active Tuberculosis (TB), mumps, and chicken pox).
- Ensure that infectious disease awareness training is provided for all OSHA Field Personnel who may be exposed to infectious diseases as a result of the work tasks they perform.
- Provide personal protective equipment (PPE), tools, and resources to ensure that the infectious disease control guidelines specified in this chapter are followed.
- Ensure that any known exposures or unsafe conditions are addressed and corrected.
- Ensure that a JHA is completed. See Appendix F: Considerations for Creating an Infectious Disease Related JHA for more information.
- An OSHA Manager will notify the RSHM if a significant infectious disease hazard has been identified.
- National Office
-
Employees
- Complete infectious disease awareness chapter training.
- Conduct a JHA prior to any onsite inspection, investigation, or evaluation.
- Utilize appropriate PPE, tools, and resources in accordance with the guidelines of this chapter.
- Report any known exposures to an infectious disease that may affect the workplace to the supervisor, including any potentially contaminated areas (e.g., vehicles and frequented rooms).
- Report any work-related infectious disease or illness in the DOL injury and illness reporting system (e.g., Ecomp) per 29 CFR 1904 Recording and Reporting Occupational Injuries and Illnesses.
- Report any notice from local health departments regarding contact tracing or office response to a potentially infectious employee (e.g., employee with active TB, mumps, chicken pox, etc.)
-
All OSHA Field Personnel:
General Contact Transmission Preventive Measures
- Practice hand hygiene.
- Cover coughs and sneezes.
Note: Wearing a mask alone does not guarantee complete coverage of coughs and sneezes.
- Maintain a physical distance from others when suspected of being exposed to an infectious disease or wear respiratory protection, as necessary. See SHMS Chapter 18: Respiratory Protection and 29 CFR 1910.134 for more information.
- Clean and disinfect high-touch surfaces regularly.
- Stay home if sick. Note: Must abide by the OSHA’s leave requirements and recommendations.
- Follow all OSHA and/or public health recommendations from other government agencies, such as CDC/NIOSH.
Note: Abiding by all OSHA and/or public health recommendations also applies to other forms of transmission of infectious diseases.
See Appendix E: CDC Standard and Transmission-based Precautions for more information.
- Management
-
Procedures
-
Hazard Assessment/Risk Assessment
A hazard assessment shall be performed by OSHA Field Personnel before performing assigned tasks and responsibilities where there is a potential for exposure to infectious agents. (See SHMS Chapter 8: Personal Protective Equipment for more information on JHAs.)
Considerations for completing an infectious disease-related JHA, see Appendix F: Considerations for Creating an Infectious Disease-Related JHA.
-
OSHA Staff Notification and Protocols for Potential Exposure
- Managers must notify their staff of potential exposure to infectious disease threats that could be spread in the workplace or developed during work.
- Managers must not provide personally identifiable information to OSHA personnel not authorized to have that information.
- OSHA Field Personnel shall notify their supervisor of a known exposure to an infectious disease so that a decision about appropriate work conditions can be made about coming into the office.
- In accordance with DOL or OSHA guidelines: If an OSHA Field Office has been potentially contaminated by an infectious agent, the responsible manager is to take appropriate steps to isolate the area and arrange for the space to either be disinfected or isolated beyond the time the infectious agent can survive.
- Managers can post notices on doors, activate a phone tree, implement telework, and increase office and vehicle cleaning procedures.
- When OSHA Field Personnel learn that they have been exposed to an infectious disease while at work, they should:
- Immediately isolate,
- Inform their supervisor (by phone or electronically (i.e., MS TEAMS or email) per Section V. Roles and Responsibilities,
- Don appropriate PPE and depart the worksite immediately (or never enter the building).
- Consider going home, if safe, to a medical facility. If possible, avoid mass transit to reduce infecting others.
- See Appendix G: Infectious Disease Exposure Assessment Flow Chart for more information.
- See Appendix H: Hierarchy of Controls for Infectious Disease for more information.
- Notify the Regional or National Office as required per Section V. Roles and Responsibilities of this chapter.
- Managers must notify their staff of potential exposure to infectious disease threats that could be spread in the workplace or developed during work.
-
Incident Reporting/Investigation Procedures
If there is an outbreak of an infectious disease among the workforce at a site where OSHA personnel are conducting an inspection, evaluation, or investigation or amongst personnel in an OSHA office that results in an infectious disease-related case, then incident reporting and investigation procedures will be conducted as outlined in SHMS Chapter 2: Safety and Health Management System: Section VII. Incident Reporting/Investigation Procedures and its Appendix C: Hazard Reporting and Incident Investigation Worksheet. A reported incident is considered a case.
Note: Seasonal Influenza is not a reportable infectious disease.
-
Emergency Response
In the event of an infectious disease emergency, such as an epidemic or pandemic, defined in IV. Definitions, refer to SHMS Chapter 7: Emergency Contingency Plan. The National Office has technical, emergency, and medical professionals as a resource to all of OSHA to assist as needed. See Section V. Roles and Responsibilities of this chapter.
-
-
Training Requirements
All OSHA Field Personnel are required to successfully complete training on the topics and details within this program. For infectious disease awareness training schedule and record retention requirements and procedures, see SHMS Chapter 2: Safety and Health Management System.
Appendix A: Guidance for Improving Air Quality in OSHA Workplaces
The Heating, Ventilation, and Air Conditioning (HVAC) systems within GSA leased/owned spaces are controlled by GSA and not OSHA. OSHA managers are encouraged to work with their GSA representatives to encourage building managers or maintenance contractors to implement the following strategies to reduce the possibility of infection via the HVAC system, as circumstances permit.
- Maintain HVAC systems, in accordance with manufacturer recommendations, including for changing filters.
- Use air purifiers with high-efficiency filters. High-Efficiency Particulate Air (HEPA) filters remove 99.97% or more of 0.3-micron airborne particles including bacteria, mold, and viruses (infectious agents).
Note: Use filters with a Minimum Efficiency Reporting Value (MERV) of 13, where possible.
- Ensure filters fit properly in the filter rack to reduce air from bypassing the filters.
- Circulate more air when the building is occupied.
- Aim for five or more air changes per hour (ACH) to reduce concentrations of indoor contaminants.
- Bring in more clean outdoor air by opening windows and doors and use exhaust fans as appropriate.
Note: Do not open windows/doors if opening them exposes OSHA personnel to the public and potential safety concerns (e.g., intruders, wild animals, etc.)
- Use portable carbon dioxide monitors to determine if appropriate levels of fresh air are being provided.
Note: Readings above 800 parts per million suggest that more fresh air may be needed in a space.
- Ensure that air purifying units are sized appropriately for the space when they are used.
- Install ultraviolet (UV) air treatment systems that do not emit ozone and ensure that they are placed in locations per the manufacturer’s recommendations.
Appendix B: Spread of Communicable and Infectious Diseases
Communicable diseases are capable of being spread from person to person. Some diseases are spread more easily than others depending on the mode of transmission (e.g., contact, fecal-oral, airborne, or parenteral) described below. Other factors that affect the risk of acquiring a communicable disease are the infectivity or ease with which the germs are transmitted and the health of the person’s immune system. People with weakened immune systems, including the elderly, chronically ill, and people taking drugs or steroids for autoimmune disease, are at higher risk of acquiring communicable diseases.
Infectious diseases can be spread through air, water, food, or soil. They can also be spread by vectors (i.e., biting insects) or by animals to humans. Infectious diseases can occur in various occupations and industries. Some infectious diseases are contagious or communicable.
Routes of Transmission: (See Section IV. Definitions to define the routes listed below.)
- Direct Contact
- Airborne Route
- Contact Route (e.g., skin)
- Droplet Route or
- Parenteral Route (e.g., bites that break the skin, needlestick or other sharps injury)
- Indirect Contact
- Fecal Oral Route (e.g., through contaminated food or water)
- Fomite Route (e.g., through contaminated equipment or laundry)
- Vector Route (e.g., through mosquito, tick, or flea bite)
For more information, see CDC’s Chain of Infection Components.
Appendix C: List of Infectious Diseases and General Resources
National Library of Medicine: National Center for Biotechnology Information:
Occupational Infections
OSHA Worker protections against occupational exposure to infectious diseases
Appendix D: Vaccines and Immunizations
CDC: Vaccine Information for Adults
Appendix E: CDC Standard and Transmission-Based Precautions
CDC recommends standard precautions and transmission-based precautions when dealing with the possibility of spreading infectious diseases in healthcare. However, these practices may be used as good practices by offices for protection against infectious diseases. Standard precautions are basic practices that apply to many settings, including healthcare and patient care. They’re based on a risk assessment and make use of common-sense practices and PPE use. Transmission-based precautions (e.g., contact, droplet, airborne) are used in addition to standard precautions for patients with known or suspected infections. OSHA’s Bloodborne Pathogens: Worker Protections Against Occupational Exposure to Infectious Diseases webpage compares the universal precautions of OSHA’s Bloodborne Pathogens standard to the CDC’s standard precautions and transmission-based precautions used by healthcare practitioners for infection control. Refer to CDC’s Infection Control Basics for greater details and the most up-to-date information on the following recommended standard precautions:
Table 1. CDC Standard and Transmission-Based Precautions:
| Hand hygiene |
|
| Environmental cleaning and disinfection |
Note: For a listing of products registered against common pathogens review the Selected EPA-Registered Disinfectants. |
| Respiratory hygiene and cough etiquette |
|
| Personal Protective Equipment (PPE): | |
| Gloves |
|
| Gowns (or coveralls) |
|
| Masks and Respirators |
|
| Face and Eye Protection |
|
Appendix F: Considerations for Creating an Infectious Disease-Related Job Hazard Analysis (JHA)
Table 2. Common Settings for Infectious Disease: Transmission and Outbreak*:
| Healthcare | Healthcare-Related | Congregate |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
*Note: Primary transmission routes of infectious diseases: Airborne, Contact, Droplet and Parenteral
Safe work practices to consider when developing a Job Hazard Analysis (JHA) to prevent and/or minimize the risk of exposure to infectious disease in preparation for field activity may include:
- Develop a written JHA prior to field activity. Refer to SHMS Chapter 8: PPE for guidance on recommended JHA formatting.
Some suggested JHA content considerations:
Work Task Potential Hazard Hazard Controls Ex: Ex: Ex: Conduct employee interviews - Being in contact with any site personnel who may have direct contact with patients being tested and/or treated
- Being in contact with any site personnel who may have indirect contact with patients being tested and/or treated
- - Conduct interviews remotely (ex. via phone, etc.)
- - Maximize physical distancing
- - Avoid direct contact and do not shake hands
- - Utilize PPE as appropriate
- Be aware of the potential for exposure to types of infectious diseases and the routes of transmission.
- Confirm and avoid potential exposure to suspected or confirmed infectious disease patients in healthcare settings.
- Determine the appropriate PPE necessary based on the activity(ies) to be performed and the potential means of exposure:
- Refer to SHMS Chapter 8: PPE for guidance.
- PPE may include goggles, disposable gloves, disposable gowns or coveralls of appropriate size, and an appropriate respirator.
- Face coverings, masks, or respirators may be used as a means of source control and should be if OSHA policy (29 CFR 1910.134, CPL 02-00-158: Inspection Procedures for Respiratory Protection, SHMS Chapter 18: Respiratory Protection, etc.) requires. OSHA Field Personnel may voluntarily use N95 filtering facepiece respirators (See 29 CFR 1910.134 Appendix D: Information for Employees Using Respirators When Not Required Under the Standard).
- Discuss the need for entry with the Area Director, prior. It is not generally necessary for OSHA Field Personnel to enter patient rooms or airborne isolation areas.
- Conduct interviews in uncontaminated areas. Interviews must not take place in a room where aerosol-generating procedures are being or have recently been performed.
- Practice physical distancing while conducting interviews with employees. Conduct interviews via phone or video conferencing (i.e. MS TEAMS, Zoom, etc.) when possible.
- Pre-plan for where donning and doffing of PPE and decontamination can be performed. (See SHMS Chapter 26: Decontamination for guidance.)
- Take the minimal equipment necessary to conduct the inspection and place cell phones and camera devices in plastic bags to prevent contamination.
- Provide a business card and request that any documents be provided via email or take photos of documents that may not be available electronically to avoid contact.
- Wash hands (and arms, if exposed) with soap and water or use hand sanitizers with at least 60% alcohol after leaving areas, touching surfaces, or removing gloves or other PPE.
- Practice contamination reduction techniques (i.e., limit surface touching, and avoid secondary or subsequent contact, especially with face).
- Discard any disposable items prior to entering a vehicle, utilize disinfecting spray and wipes to disinfect equipment, and clean and disinfect the vehicle following use. Be sure to follow instructions for disinfecting, i.e., appropriate contact time.
- Stop activities and consult with a supervisor. If conditions arise that could create an increased risk of exposure to infectious disease, OSHA personnel must remove themselves from the potentially hazardous condition.
Appendix G: Infectious Disease Exposure Assessment Flow Chart
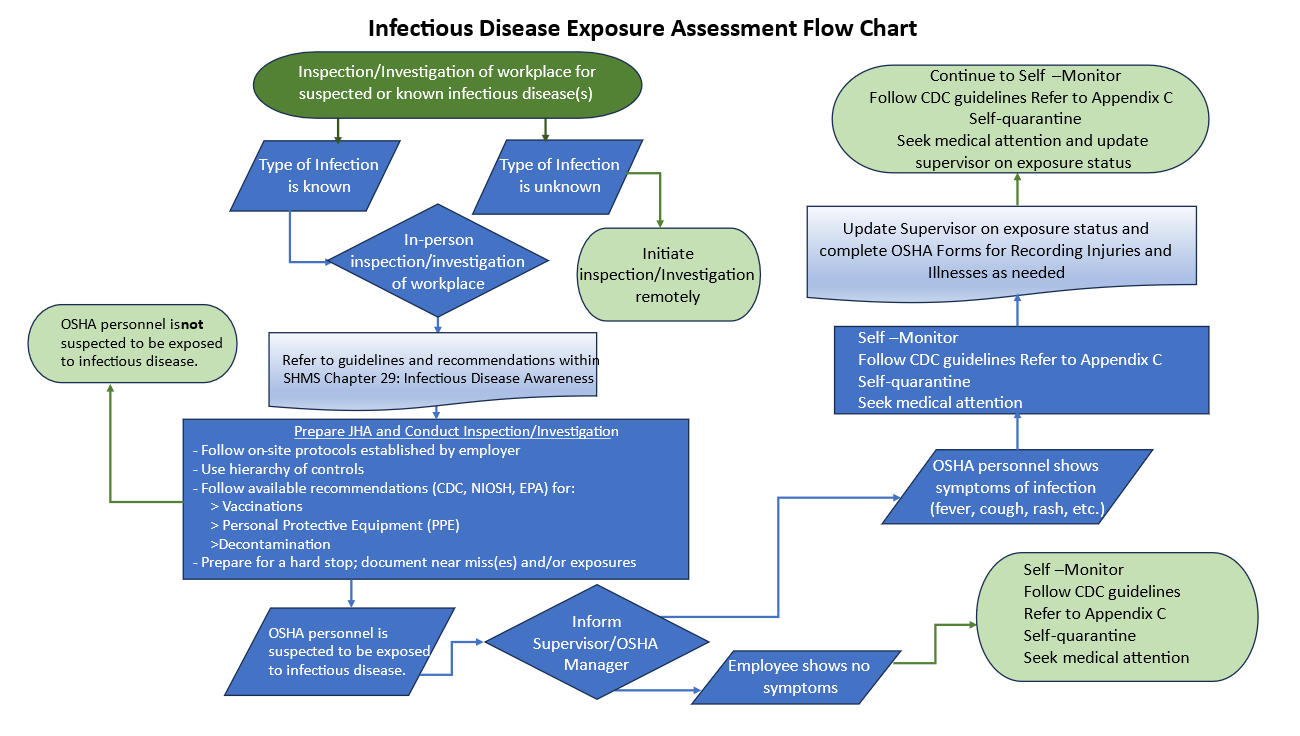
Figure 1. Infectious Disease Exposure Assessment Flow Chart (.pptx format)
Appendix H: Hierarchy of Controls for Infectious Diseases
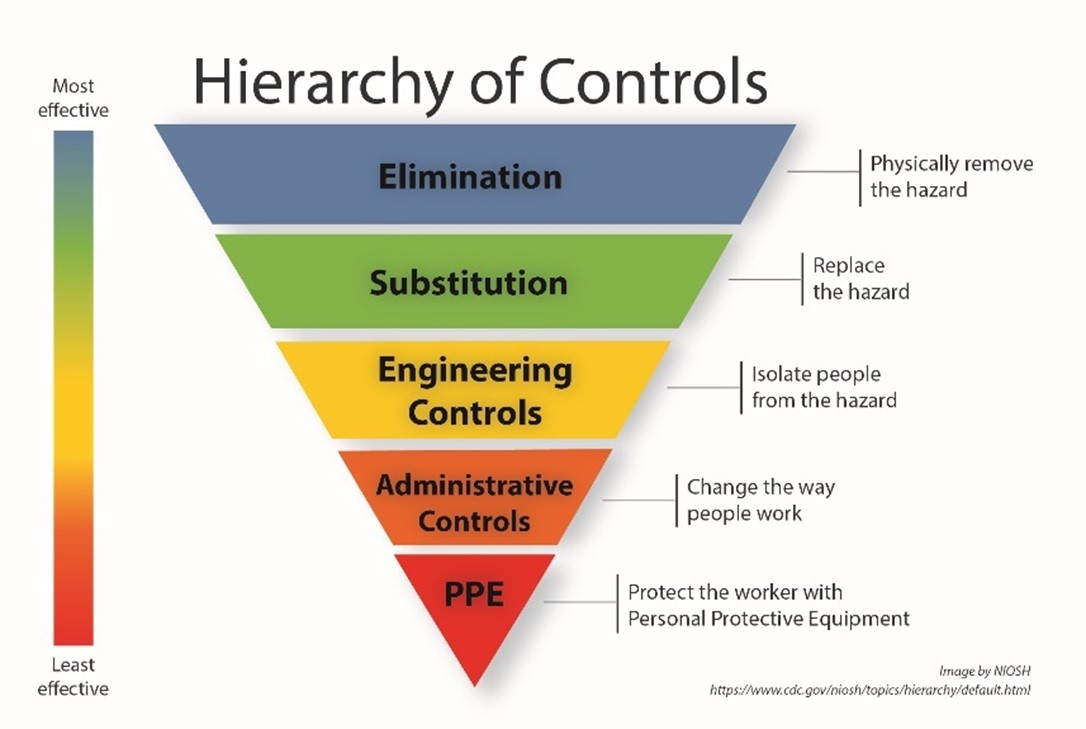
Figure 2. Hierarchy of safety controls
Controlling exposures to hazards in the workplace is vital to protecting workers. The hierarchy of controls is a way of determining which actions will best control exposures. The hierarchy of controls organizes hazard controls from most effective to least effective in reducing risk in the workplace.
Hierarchy of Controls for Infectious Disease:
-
Elimination:
Removes the hazard at the source. It is the preferred solution to protect workers because no exposure can occur.
- Whenever possible, avoid exposure to infectious diseases by working remotely. Managers should actively encourage potentially contagious employees to stay home.
- Avoid worksites with known outbreaks; if possible, conduct site visits and interviews via phone/video conferencing/remotely. Infectious disease outbreaks may be tracked by the local health department and CDC depending on the disease. Personnel visiting worksites should check to see if available content for information on local outbreaks of infectious diseases is available on CDC’s Current Outbreak List.
-
Substitution:
Using a safer alternative to the source of the hazard. Effective substitutes reduce the potential for harmful effects and do not create new risks.
Vaccination: Personnel should follow current OSHA policy on vaccinations (OSHA personnel can refer to the DOL Intranet). The CDC also provides recommendations on vaccination schedules. See Appendix D: Vaccine and Immunization for more information on the types of vaccines and CDC recommendations.
-
Engineering Controls:
Reduce or prevent hazards from coming into contact with workers. Engineering controls can include modifying equipment or the workspace, using protective barriers, ventilation, and more.
- Ventilation: Improved airflow in buildings can help protect occupants from respiratory infections. For example, installation of specialized negative pressure ventilation in some settings, such as for aerosol generating procedures, can be helpful. Facility managers are encouraged to work with building maintenance contractors to implement the strategies listed in Appendix A: Guidelines for Improving Air Quality in OSHA workplaces.
- Protective Barriers: Barriers such as, but not limited to, Plexiglass, Sneeze Guards, or Shields, create a barrier between workers and the infectious disease hazard.
-
Administrative controls:
Establish work practices that reduce the duration, frequency, or intensity of exposure to hazards. Administrative controls require significant and ongoing effort by workers and their supervisors. They are useful when employers are in the process of implementing other control methods from the hierarchy. Additionally, administrative controls and PPE are often applied to existing processes where hazards are not well controlled.
- Medication: If available, medication may reduce the possibility of infection, known as primary prevention. A medical professional should guide the use of medications as prophylaxis to prevent disease. All of these prescription medications should be administered and taken under the direction of a licensed healthcare provider.
- Testing: Early identification of an infection, through regular testing, can control the spread to others. The goal of screening for infectious disease is to identify the cause of their related symptoms and treat people before they have serious health complications.
- Symptom Screening: In certain circumstances, such as during outbreaks of infectious disease (local or global), the common signs and symptoms of the specific illness will be communicated to OSHA personnel by the DOL or OSHA leadership with a reminder to stay away from the workplace if they or someone is experiencing these symptoms.
- Signage: Signs such as those alerting the population not to enter if they show signs of infectious disease and notifying workers of the policy to work from home if they are exhibiting symptoms may be used as administrative controls.
- Cleaning and Disinfection: Work surfaces should be cleaned with an agent that is known to remove the transmissible virus. Workers should be aware that such agents often require “stay times” typically 30 seconds to 2 minutes depending on the product, in order to be effective at killing the virus.
-
Personal Protective Equipment (PPE):
Should be the last method considered for protection against infectious disease. PPE relies on the individual to correctly use assigned protection and is subject to human error. Examples of PPE used may include:
- Face masks: If NIOSH-approved respirators, including filtering face-piece devices (commonly called N95s or N99s) are required to be used in the workplace, the requirements set forth in OSHA’s Respiratory Protection Standard, 29 CFR 1910.134, must be followed.
- Gloves: Workers should be taught how to don and doff gloves correctly to minimize transmission of infectious disease. Gloves should be replaced whenever there is a tear or break in the glove.

